Of the many pains that can effect the head and neck, perhaps the most confusing and difficult to diagnose are a group of maladies called Neuropathic Orofacial Pain Disorders. These neuropathic pain disorders are often chronic and arise from the brain and nerves of the head, face and neck.
If you have experienced the frustration of having a toothache or face pain and, after seeing many doctors, still don’t know where the pain is coming from, you may be suffering from a neuropathic pain disorder. In the past, many patients were told that these types of pain were of psychological origin, but recent research has shown that most of these pains have physical origins and can be managed effectively when properly diagnosed.
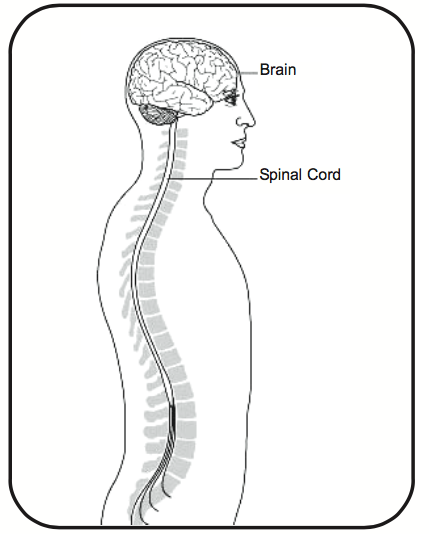
The nervous system can be divided into two general parts: the central portion, which includes the brain and spinal cord, and the peripheral part, which includes the nerves that go to such outlying areas of the body as the arms, legs, trunk, face and teeth. The peripheral nerves involved with neuropathic pain provide sensations from various stimuli, such as touch, heat, chemicals or pain, from a particular area of the body. The pain nerves course their way back to the spinal cord where they connect to a second nerve which extends up the spinal cord to the brain where the information is processed. In the brain, a different nerve continues to carry the message to other parts of the brain where the message is actually interpreted as pain. The brain has many complex chemical mechanisms to either increase or decrease the pain-related information streaming into it.
If a peripheral nerve is injured, for example a tooth has a nerve injury from decay and subsequent root canal treatment, one might correctly expect that the tooth would be sore for several days. Sometimes, however, the tooth continues to hurt for months and even years. Even more perplexing, the tooth may be extracted and can continue to hurt as if it were still there.
 Science has shown that after a peripheral nerve is injured, there can be permanent changes in the area where that nerve was first injured, in the area where it meets the spinal cord, and further up the chain of nerves into the brain. These changes can result in continued pain, despite normal healing in the area of the tooth. Research has also shown that the nervous system can undergo changes both in the peripheral portion and even more surprisingly, in the central portion so that the persistent pain may come from either one or both parts. This is a phenomenon called “plasticity” which means that the nervous system can be altered so that non-painful signals such as touch and pressure are interpreted by the brain to be painful. The brain then continues to perceive that the area that was first injured is the area that is painful even though it has healed.
Science has shown that after a peripheral nerve is injured, there can be permanent changes in the area where that nerve was first injured, in the area where it meets the spinal cord, and further up the chain of nerves into the brain. These changes can result in continued pain, despite normal healing in the area of the tooth. Research has also shown that the nervous system can undergo changes both in the peripheral portion and even more surprisingly, in the central portion so that the persistent pain may come from either one or both parts. This is a phenomenon called “plasticity” which means that the nervous system can be altered so that non-painful signals such as touch and pressure are interpreted by the brain to be painful. The brain then continues to perceive that the area that was first injured is the area that is painful even though it has healed.
The pains that result can vary, but often times will have several qualities that distinguish them from other pains. Often the patient complains that the pain just happens by itself, or that light touch, or hot or cold stimulation triggers it. Sometimes it is difficult for the patient to figure out just where the pain is coming from. It may seem that there is a general area that is painful. The pain can vary from a general nagging dull ache to a sharp, stabbing, shock-like pain; we call this kind of sharp pain “paroxysmal”.
Getting help/What to expect
 Patients with neuropathic orofacial pain often visit many doctors and undergo many tests, all of which are negative. Even more frustrating and upsetting to the patients is that they undergo useless treatments. In the mouth, this may include gum surgery, root canal and even extraction, which often results in only temporary relief, no relief at all, or in many cases an increase in pain.
Patients with neuropathic orofacial pain often visit many doctors and undergo many tests, all of which are negative. Even more frustrating and upsetting to the patients is that they undergo useless treatments. In the mouth, this may include gum surgery, root canal and even extraction, which often results in only temporary relief, no relief at all, or in many cases an increase in pain.
Persistent pain should be evaluated by a physician, usually a neurologist or anesthesiologist specially trained in pain management or, in the case of the head and neck, by an orofacial pain specialist. The doctor will perform a comprehensive evaluation, which may include a thorough history, examination, and diagnostics tests.
The history should include recording the exact nature of the pain and other symptoms you may have, the history leading up to the persistent pain, previous doctors seen, past treatments and their results, and list of medications taken with their effectiveness and/or side effects.
The examination should consist of touching different areas of the head, neck and inside the mouth, measurements and evaluation of the jaw, head and neck, and gentle provoking of the pain. This can be with light touch, cold or heat or heavier touch. The doctor may also perform some simple neurological tests.
After this, Dr Hung may decide to order diagnostic tests which could include magnetic resonance imaging (MRI), computer assisted tomography (CT) or other radiographs (X-rays). In addition your doctor may want to order blood tests, urinalysis, and other tests. These tests are used to make sure that there are no other factors that may be contributing to the neuropathic pain. To discover if the pain is peripheral or central (or both), the doctor may use a series of diagnostic injections, usually with a local anesthetic, similar to what might be done when you have a tooth filled. By “numbing” the nerves in the peripheral part of the nervous system and determining its effect on the pain, important information can be learned and may help in planning a more effective treatment. A battery of psychological tests may be appropriate since anxiety and depression often accompany persistent pain.
Depending on the complexity of the problem, the Dr Hung will decide which of the diagnostic tests are appropriate. After piecing together the results of the history, examination, and diagnostic tests, the doctor will make a diagnosis and recommend a treatment strategy. Sometimes treatment is done on a trial basis and several treatments may be attempted before an effective approach is found. In addi- tion your doctor may enlist the help of several professionals to provide what is called a “multidisciplinary approach”.
Common Neuropathic Orofacial pain Disorders and their treatments
Trigeminal Neuralgia
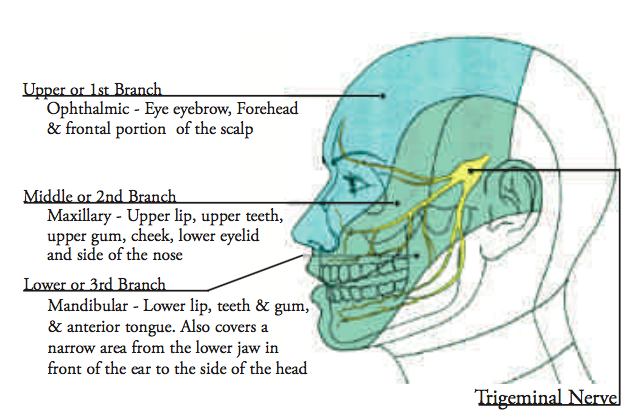
Of the neuropathic pain disorders, perhaps the best known is Trigeminal Neuralgia (TN). It often appears suddenly as a sharp, shooting, lightning-like pain lasting a few seconds. There may be a specific trigger area that, when touched, causes the pain to occur. Patients are often unable to shave, comb their hair, or touch their face for fear of triggering the pain. Sometimes the pain is triggered by slight movement of the affected part of the face. The disorder is more common after age 50 but can occur at any age.
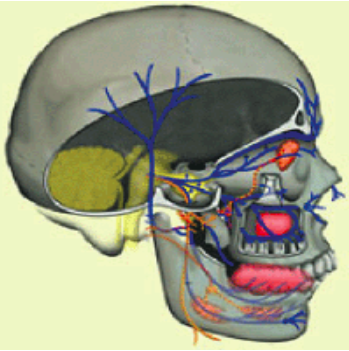
The trigeminal nerve is the main nerve that provides sensation to the face. The nerve is divided into three branches on either side of the face and the pain of TN usually follows one or more of these branches. The cause of TN is often unknown, but many doctors and researchers feel that at least in some patients, there may be a compression of the trigeminal nerve by an artery or vein within the brain. Also, patients with tumors in the brain and with Multiple Sclerosis may suffer from TN-like pain. Therefore, all patients need to be carefully evaluated before starting therapy. There are also several other, less common neuralgias involving other nerves of the face.
 The first line of treatment for TN is usually with one of a group of medications called “anti-seizure medications”. Often patients are started on a very low dose which is increased to the lowest effective dose. It can take several weeks before it can be determined if a particular drug is effective. Some of these medications require periodic monitoring of the blood to avoid undesirable side-effects. There are several different medications available so that inadequate responses or side- effects from one medication can lead to trials of other drugs.
The first line of treatment for TN is usually with one of a group of medications called “anti-seizure medications”. Often patients are started on a very low dose which is increased to the lowest effective dose. It can take several weeks before it can be determined if a particular drug is effective. Some of these medications require periodic monitoring of the blood to avoid undesirable side-effects. There are several different medications available so that inadequate responses or side- effects from one medication can lead to trials of other drugs.
When medication is ineffective, surgery or special injections (blocks) may be recommended. Surgery is generally performed by a neurosurgeon while blocks are performed by specially trained anesthesiologists. The injections are aimed at temporarily or permanently blocking the effected branch of the trigeminal nerve. Patients should exercise caution before undergoing these procedures because permanent numbness and continued pain can occur.
One surgical treatment, called microvascular decompression (“MVD”), is designed to take the pressure off the trigeminal nerve by placing a small cushion between it and a blood vessel.
There are four other blocking procedures that treat the nerve in order to interrupt the pain. Three of these procedures are done through-the-cheek. They are: Balloon Compression, Glycerol Injection, and Radiofrequency Lesioning. A relatively new procedure is Radiosurgery (Gamma Knife), which uses highly focused beams of radiation to treat the nerve.
Of course, if the neuralgia-like pain is from the pressure of a tumor, this will likely be treated by surgery, radiation therapy and/or other forms of treatment appropriate for the particular pathology.
As with treatment for any disorder, the patient should have a frank discussion of the risks and benefits of the chosen treatment as well as treatment alternatives. It is always advisable to seek a second opinion.
Pre-Trigeminal Neuralgia
Some patients will experience a vague, deep dull achy pain in the face or teeth. It may be constant or on and off. Local anesthesia often temporarily relieves the pain. This pain eventually develops into TN and is called “Pre-Trigeminal Neuralgia”. This is treated with the same medications as TN. This pain can be difficult to diagnose but becomes evident as it presents itself in the classical form of TN.
Atypical odontalgia (phantom tooth pain)
As previously mentioned, some patients develop persistent tooth pain and go from dentist to dentist only to be told there is nothing wrong with their teeth. This pain often, but not always, follows a dental procedure such as a root canal or filling. Unfortunately, many patients undergo unnecessary root canal treatment, gum surgery, and even extraction in a vain attempt to treat their pain. The pain actually starts at the peripheral nerves that go to the teeth and in some cases can progress to changes in the central part of the nervous system that then senses tooth pain.
When the pain comes from the part of the nerve close to the teeth or gums, injections of local anesthetics and steroids may be effective. Some patients find relief by applying specially prepared creams with various combinations of medications mixed in them. In patients where the pain is central rather than peripheral, medication taken by mouth may be needed on a daily basis. These often include antidepressants and anti- seizure medications and in some cases even narcotics.
Chronic Regional pain syndrome
Chronic Regional Pain Syndrome (CRPS) often results from peripheral nerve damage that causes changes in the peripheral and central parts of the nervous systems, similar to what is seen in atypical odontalgia. The difference with this kind of pain is that the sympathetic nervous system is involved. This is the part of the nervous system that, among many other things, controls blood flow. So, in addition to the pain, the patient often complains of a cold feeling because the blood vessels in the area narrow. The pain is often described as burning and is triggered by light touch or other stimulation. CRPS most often occurs in the arms and legs but can occur in the face.
Treatment usually consists of antidepressants, pain medication, and medications used to control blood pressure. Physical therapy aimed at restoring the affected area to normal function may be helpful. Sometimes a series of injections in certain of the main nerve intersections or “ganglia” are helpful, particularly in the early stages of the disorder.
When all else fails, there is a surgical procedure that treats specific nerves that surround the area. The procedure is called “sympathectomy”. But, as with any surgery for chronic pain, proceed cautiously.
Brochure – “Toothaches of Non-dental Origin”
In Conclusion
Treatment of neuropathic pain disorders may require considerable patience to eventually control the pain because the first method of treatment, or even the second, may not be successful. Through careful scientific research we are discovering new treatments all the time and more doctors are learning about Neuropathic pain Disorders. Try to avoid being discouraged if you don’t get well immediately. Maintain close communication with Dr Hung in a cooperative manner in an effort to obtain the most effective results.

