SNORING AND SLEEP
Sleep apnea has recently been associated with risk factors for serious medical conditions such as stroke, diabetes, cardiovascular disease including high blood pressure, heart arrhythmias, heart attack, and even erectile dysfunction.
Also, many motor vehicle accidents are attributed to day time sleepiness as a result of sleep apnea.
Sleep apnea is very common and is estimated to affect as many as 18 million Americans or about 1 in every 15 individuals. Of the three types of sleep apnea (obstructive, central and mixed) obstructive is the most common. In central sleep apnea, the airway is not blocked, but the brain fails to tell the body to breathe.
SIGNS OF SLEEP APNEA
- Gasping, choking or snorting during sleep
- Feeling sleepy or tired, in spite of a full night’s sleep
- Waking up tired or with a headache
- Falling asleep in inappropriate situations (movies, church, sitting quietly) or without meaning to sleep
- Problems with memory and concentration
- Being ill-tempered or irritable
DIAGNOSIS
Your Medical doctor will inquire about your sleep problem and examine you. Oftentimes, an overnight sleep study will be recommended. This study helps determine if your snoring is sleep apnea, and its severity.
History – Your doctor may inquire about how long you have snored, your sleep habits, lifestyle and work issues, medical conditions, medications used, daytime sleepiness, and the impact snoring has on you and those who live with you.
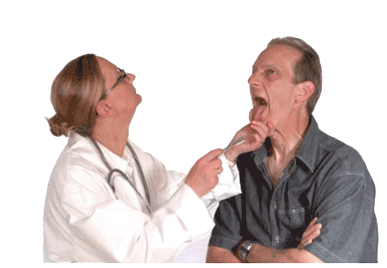 Physical Exam – Your doctor may look in your mouth, nose and throat, check your weight, blood pressure, pulse, and neck size. Lab tests and imaging may also be ordered to properly assess your airway.
Physical Exam – Your doctor may look in your mouth, nose and throat, check your weight, blood pressure, pulse, and neck size. Lab tests and imaging may also be ordered to properly assess your airway.
An examination may show a decreased space at the back of your mouth, where your throat begins.
Sleep Study – This is usually performed in a sleep center and provides the most information about how you breathe when you are asleep. The sleep center may measure your breathing, heart rate, oxygen saturation, muscle activity, and other functions. Recently, at-home instruments have become available that measure some of these functions in a more normal and comfortable atmosphere-your own bed.
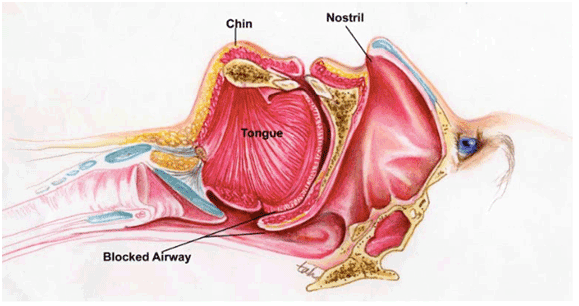
ANATOMY OF BREATHING
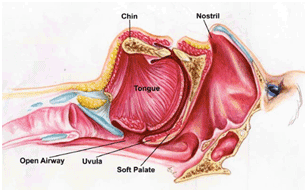
Air travels through nasal passages and the throat. Normally these passages are open enough to allow air to flow freely and breathing is normal. The passages can become constricted causing snoring; if they become sufficiently narrowed or blocked, apnea can result. The ideal mode of breathing is through the nose. Under ideal conditions, air passes through the nose into the oral airway and into the lungs. This mode of breathing warms, humidifies and filters the air thus improving the available oxygen.
Nasal Structures – The inside of the nose is divided by a septum and along the inside walls of the nose are ridges called turbinates. A deviated septum can make breathing through the nose more difficult. The turbinates can become swollen decreasing the passage of air through the nose. Other nasal obstructions, such as polyps, can also make nasal breathing more difficult.
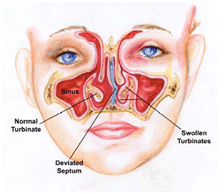
Often people who have chronic difficulty breathing through their nose will become mouth breathers. Any obstruction to normal nasal breathing may need to be evaluated and possibly corrected in order to help treat a snoring or sleep apnea problem.
Throat Structures – At the back of the mouth is the soft palate, uvula, tonsils, and the rear portion of the tongue. Muscles hold these structures in position. When sleeping, these muscles relax, but usually hold the structures firm enough to keep the airway open.
If the airway is already narrow or if these structures become enlarged, it can temporarily close the airway, leading to sleep apnea.
WHAT YOU CAN DO TO IMPROVE SLEEP?
CHANGING CERTAIN HABITS MAY RESULT IN BETTER SLEEP. WHILE THESE CHANGES MAY TAKE TIME AND EFFORT, THE IMPROVEMENT WILL BE WORTH IT.
SLEEP ON YOUR SIDE – If you sleep on your back, gravity may pull the tissues of your throat down, blocking your airway. Sleeping on your side may help keep your airway open.
LOSE WEIGHT – Folks who are overweight often have bulky and excess tissues in their throat which can make snoring and apnea worse. Your physician can help you develop a plan to lose weight and keep it off.
EXERCISE – Do not exercise within three to four hours of bedtime.
AVOID ALCOHOL AND MEDICATIONS – Alcohol and some medications like sleeping pills, some antihistamines, and sedatives can relax the muscles of your throat which may worsen snoring and apnea. Avoid alcohol three to four hours before sleep and talk to your doctor about medications you take that can impact snoring and apnea.
CLEAR YOUR NOSE – A clogged nose won’t let air in as easily. Allergies and sinus problems can also contribute to difficulty breathing through your nose. Nasal strips can help make breathing easier. There are also nasal rinses and sprays that can make nasal breathing easier. Your doctor will recommend these if they are appropriate.
DON’T EAT NEAR BEDTIME – Allow three to four hours between eating and bedtime.
MANAGEMENT
Many treatment options are available for snoring and sleep apnea. The recommended therapy for sleep apnea depends on its severity, which is usually determined by a sleep study or examination.
CPAP – Continuous Positive Air Pressure (CPAP) consists of a small device that pumps air into a mask that is held over your nose by a strap. The air pressure holds the airway open, allowing you to breathe more easily. CPAP is sometimes combined with other treatments. For most people with sleep apnea, CPAP will be the first type of treatment recommended.

Types of CPAP – Basic CPAP keeps constant air pressure on the airway all night. A bi-level CPAP senses when you breathe in and out and automatically adjusts the air pressure accordingly. An autoCPAP machine automatically responds to changes in body position, how deeply you are breathing, and if you are snoring. Some of these devices also humidify the air so the tissues do not dry out. Your doctor will assist you in deciding which type of device is best for you.
Compliance with CPAP – It takes most people some time to get used to the CPAP. Many of the problems can be overcome by changing the type of machine you use, modifying the mask, or other aspects of this treatment. However, some people, no matter what they try, cannot tolerate using CPAP.
Oral Appliance Therapy – Provides an alternative to CPAP and is primarily used for snoring or mild to moderate sleep apnea. Custom fabricated oral appliances hold the lower jaw and tongue forward to create more space in the back of the mouth and throat increasing the airway space and prevent the tongue and lower jaw from collapsing back causing airway obstruction.
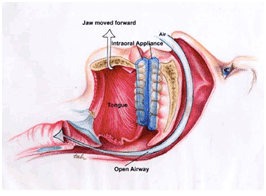
These devices generally work well but, like CPAP, are not for everyone. A specially trained dentist can help you determine if you are a good candidate for an oral appliance. Like CPAP, oral appliances require getting used to and they will sometimes need to be adjusted to determine the optimum position for each patient. These appliances require maintenance and follow up visits to make sure they continue to fit correctly and help you breathe better.
These oral appliances can cause some patients to develop sore or painful jaw muscles or jaw joints, have difficulty putting their teeth together when they remove the appliance, and in some cases develop changes in the way the teeth fit together.
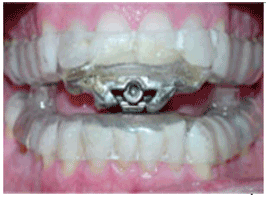
Examples of intraoral appliances to treat obstructive sleep apnea
Surgery – There are several surgical options but all are aimed at opening the airway by removing tissue at the back of the mouth and in the throat.
UPPP – Uvulopalatopharyngoplasty is the most common surgery for sleep apnea. It removes the uvula, a portion of the soft palate, tonsils and other tissue. It is major surgery and has risks and complications, as would any surgery.
LAUP – Laser-assisted uvulopalatoplasty is a method of removing a portion of the soft palate and the uvula. It usually requires several visits in the doctor’s office and can be effective for snoring and mild sleep apnea. There are potential risks and complications associated with this procedure.
RFA – Radiofrequency ablation uses radio waves to shrink the nasal turbinates or uvula, surrounding tissues and sometimes the back of the tongue.
Jaw and/or tongue surgery – There are some procedures which surgically reposition the jaw and/or tongue to open the airway.
Pillar Procedure – Tiny polyester implants are placed in the soft palate and over time these cause stiffening of the tissues. This can reduce tissue collapse that leads to snoring and obstruction of the airway.
Precautions about Surgery for Snoring or Sleep Apnea – There are some things to keep in mind if you are considering surgery to help reduce your snoring or sleep apnea. There is no guarantee that surgery will resolve your symptoms. You may still need to use CPAP or an oral appliance to adequately control your symptoms. Over time, your symptoms may return. The removed tissues may grow back or the remaining tissues may become flabbier causing a return of your symptoms. Surgery is usually considered as an option for severe sleep apnea or when other, less invasive methods have not provided adequate symptom relief.
Above information as courtesy of the American Academy of Orofacial Pain
